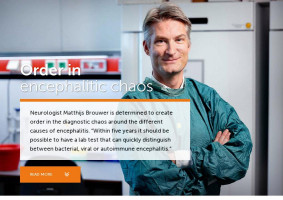
Is it bacteria? Is it a virus? Or is it the immune system gone astray? When it comes to a serious inflammation of the brain tissue, an exact diagnosis is notoriously difficult. “In half of the cases presented in the hospital, the exact cause of encephalitis remains unclear,” says neurologist Matthijs Brouwer. “But an exact diagnosis is crucial when you want to give the best treatment. Currently, one in six patients with encephalitis dies. This is probably at least partly due to a delay in treatment. As long as the exact cause of the problem is unclear, no specific, efficacious treatment can be given.”
During a pilot study at several Dutch Emergency Rooms (ERs), Brouwer and his colleagues noticed that the cases where encephalitis is caused by an autoimmune disease, in particular, are recognized late, if at all. “This is the group with the worst prognosis,” he says. “Frequently, the diagnosis is a matter of trial and error. If a patient improves on antibiotics, it was likely an infection caused by bacteria. If anti-viral drugs improve the situation, it was probably a virus. But to me, that feels a bit like practicing medicine in the dark.”
Torture
To shed light on this diagnostic chaos, Brouwer received a €2 million Consolidator Grant from the European Research Council, which he wants to use to improve the diagnosis of encephalitis through innovative diagnostic methods. “In our research project IPACE – ‘Improving Prognosis by Using Innovative Methods to Diagnose Causes of Encephalitis’ – we intend to ‘torture the cerebrospinal fluid (CSF) on the cause of encephalitis until it confesses’,” Brouwer explains. “And we’re taking four different approaches for this.”
Genetic profiles
As a first strategy, Brouwer will genetically sequence the cells he will extract from the CSF, to look for cell types that are associated with either bacterial or viral infections, or cell types that suggest a deranged immune reaction. “This single-cell sequencing has never been done before in the CSF of encephalitis patients,” says Brouwer, “but it can potentially teach us a great deal.”
Wisdom of hindsight
In a second approach, Brouwer intends to benefit from the wisdom of hindsight. “If we sequence the blood of patients, using phage display sequencing, weeks after the initial inflammation has occurred, we can identify which type of virus was the cause in approximately 40% of viral encephalitis cases. Learning this afterwards may help us to narrow our diagnostic scope for future acute phases too.”
Metabolic fingerprint
Brouwer hopes to find a third clue in the metabolites and lipids that are formed in the blood in the patients’ CSF. “Different types of encephalitis may result in subtle differences in the chemical composition of the blood and the cerebrospinal fluid as well,” says Brouwer. “By looking at the exact composition of these fluids, we hope to recognize patterns that are associated with one type or another.”
Auto-antibodies
Last, but certainly not least, Brouwer intends to look for so-called auto-antibodies. “The group with an auto-immune form of encephalitis is the hardest one to recognize. Hopefully we find some specific clues in the immune system that can tell us at an early stage that we don’t need to administer antibiotics or anti-viral drugs, but that we should rapidly aim for better control of the immune system with anti-inflammatory treatment.”
Smart lab test
Every year, Dutch ERs see at least 5,000 patients with suspected encephalitis. About 1,000 of those are diagnosed with a true inflammation of the brain and of that 1,000, more than 150 die. “A lot can be gained if we can improve the early diagnosis in these patients,” says Brouwer. “During the IPACE project, I hope to take the first steps towards setting up a smart lab test; one that can easily pick the right clues from the blood or the CSF of these patients, and then instantly reply with the best therapy. ‘Fluid in, diagnosis out’, so to speak. I truly believe that we can set such an innovative, automated diagnosis in motion. Of course, the practical realization of the actual analysis, as well as the realization of the lab test itself, will take longer. We will probably need to cooperate with commercial partners on that part.”
International collaboration
In his project, Brouwer will also collaborate internationally with colleagues in the UK, Denmark and Zambia. “The incidence of infections of the central nervous system is substantially higher in African countries compared to Europe. For example, south-east Africa has a ten- to twenty-fold higher incidence of encephalitis. A country such as Zambia will therefore potentially benefit a lot from a simple test to improve diagnoses and thus treatment. At this stage we should analyze a broad range of patients to ensure that we will ultimately have a test that can be used all over the world and that will benefit everyone who suffers from encephalitis.”
Photography: Digidaan