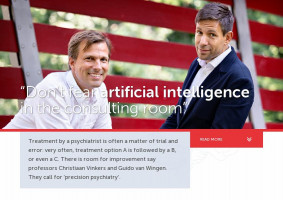
“At first glance, there is quite a big difference between psychiatry and the rest of medicine,” says Guido van Wingen, Professor of Neuroimaging in Psychiatry at Amsterdam UMC. “Every doctor tries to objectify in the consulting room. Based on the symptoms a patient presents, they request lab tests or imaging techniques, after which a treatment is implemented that is as evidence-based as possible. Psychiatry often has a harder time for that matter. In fact, there isn’t much more to go on than the patient’s information. And that story is, by definition, subjective.”
Illusion of objectivity
Professor of Stress and Resilience in Psychiatry at Amsterdam UMC, Christiaan Vinkers acknowledges this difference, although he also likes to emphasize that his fellow specialists in other fields often rely on what he calls ‘the illusion of objectivity’. “Of course, the level of evidence in other fields is also open to criticism, but it is true: while an oncologist has tumor markers or other blood values to hold onto, psychiatry has far fewer objective points of reference,” he says. “The well-known psychiatrist’s handbook, the Diagnostic and Statistical Manual of Mental Disorders (DSM), does offer classifications of disorders such as depression, but those classifications are very coarse at best. Depression is enormously heterogeneous in clinical practice; there is a wide range of triggers and manifestations. The problem can arise from childhood traumas, but it can arise from metabolic problems as well. Inflammation associated with obesity can also cause depression. So, in order to better help an individual patient in the future, there is a need to better understand where all this heterogeneity comes from.”
Trial and error
The consequences of this lack of objectivity are sometimes distressing, Van Wingen believes. “Unfortunately, a treating psychiatrist cannot predict whether a treatment will be successful. As a result, a treatment process often follows in which the right treatment is sought through trial and error.”
Just as distressing, according to Vinkers, is the lack of interest from society, and thus from policy, for this issue. “The level of investments in the Netherlands to advance the field of psychiatry is frankly quite disappointing,” he says. It is therefore time for an innovative approach, the two professors state almost in chorus, and that is called: precision psychiatry.
Big data
To be able to help an individual in a more tailored way, Van Wingen says it is first necessary to lump as many psychiatric patients as possible together. “If you conclude that psychiatry has not yet succeeded in recognizing sufficiently clear patterns in the heterogeneous patient population, then perhaps we should call in the help of artificial intelligence. For example, if we enter all the people with depression into a large database, including all their characteristics imaginable plus the medication they are taking, whether it has helped or not, then it might just be possible that a computer does see a pattern.”
Mysterious shrink
Vinkers also sees the great potential added value of artificial intelligence in the psychiatric practice, although he foresees resistance on the floor. “The average psychiatrist – including myself – often reckons they have a good clinical view and experience. But I would also like to call on my colleagues not to overestimate themselves. We should not be narrow minded, but be open for new technology that can help us. So don’t be afraid of artificial intelligence in your consulting room. Be curious,” he urges his colleagues. “In the rest of medicine, we are already much more used to allowing external variables into the consulting room. The psychiatrist is used to relying on their own judgment. But in doing so, we’ve also pretty much entrenched ourselves in a battle of directions. Where one person firmly believes in biological psychiatry, another is primarily convinced of the psychological approach. We need to listen to each other better, learn to speak each other’s language, and above all we have to learn to think outside the box.”
A support system rather than a decision machine
Van Wingen also underlines that artificial intelligence should never be more than a support system, and not looked upon as a ‘decision machine’. “Like anywhere in medicine, only the clinician knows the context, but they can be assisted by patterns that a computer recognizes and they don’t.” The potential gains are enormous, Van Wingen believes. “When we feed the computer with images from the MRI or an EEG on an experimental basis, we can already predict with an accuracy of 80% whether, for example, antidepressants or electroconvulsive therapy will be successful,” he says. “Artificial intelligence can also potentially be very helpful in stopping medication in a timely manner,” adds Vinkers. “In the Dutch TEMPO project, for example, we are investigating whether, and how best, to phase out the use of certain drugs. I firmly believe that artificial intelligence can also find indications for ‘phasing out’ or ‘continuing’ that we haven’t recognized yet.”
N-of-1, a study performed on an individual patient
In addition to this ‘knowledge from the great heap’, the two professors also foresee a lot of added value on the road to precision psychiatry in an approach that is at the completely opposite end of the spectrum: research based on N-of-1 trials. “If you dare to see a patient as their own research group, you could, for example, evaluate much sooner whether a new drug is effective,” says Van Wingen. “As a practitioner, realize that you are often wandering in the dark and therefore dare to evaluate sooner whether a certain choice has been the right one.”
Culture change
“The road to precision psychiatry will require a cultural shift,” Vinkers foresees. “But if we, as academic research, collaborate closely with clinical practice, I think that change can happen.” Van Wingen agrees: “I have actually seen this happen in practice at an external clinic. There, they investigated whether patients respond better to antidepressants when prescribed based on an EEG. And when, after the official study period, they were forced to go back to the standard way of prescribing without an EEG, they didn’t want to do that anymore.”
There’s work to be done, then, in the area of collaboration between disciplines, Van Wingen concludes. “It requires investments in psychiatry, which can help clinical practice. Those investments may well bear fruit in the not-too-distant future.”
Photography: DigiDaan